A defect in a DNA repair system may cause some leukemia patients to relapse sooner, according to new research published in the online edition of Nature Medicine.
Researchers at St. Jude Children's Research Hospital, in Memphis Tennessee, discovered recently that some young patients treated with common chemotherapy drugs for acute lymphoblastic leukemia (ALL) will experience a rapid relapse due to the genetic defect.
The finding may enable doctors to identify these patients earlier and seek more tailored therapies that could improve the patients' chances of survival. The investigation focused on a protein called MSH2, which is involved in the repair of defective DNA.
DNA, which carries instructions for building proteins necessary for life, is occasionally mistranslated. Repair proteins help correct such mistakes. But among certain leukemia patients, the repair proteins themselves are defective, due to a genetic defect. As it turns out, the defect also affects the effectiveness of chemotherapy drugs used to treat the cancer.
About 90% of children treated for ALL at St. Jude's are now cured of the disease. About 11% of children diagnosed with ALL have the genetic defect, which apparently accounts for the small percentage of children who are not cured by treatment with drugs known as thiopurine medications.
Children with the DNA repair defect quickly develop resistance to these drugs, which work in part by enlisting the aid of natural DNA repair mechanisms. "If confirmed, this work suggests a patient's MSH2 status might someday be used to guide treatment," said Barthelemy Diouf, Ph.D., one of the study's authors.
About 3,000 young patients are diagnosed with ALL each year in the U.S. The present work was informed by the observation that ten years after diagnosis children with low levels of the MSH2 protein were less likely to have survived, and more likely to have suffered a relapse of their leukemia, than children with normal levels of the repair protein. Because low levels of the protein do not impact the effectiveness of other drugs, identifying children with the defect may help improve their odds of survival. "In the future, we may want to intensify use of other therapies," said William Evans, Pharm.D., the paper's senior author.
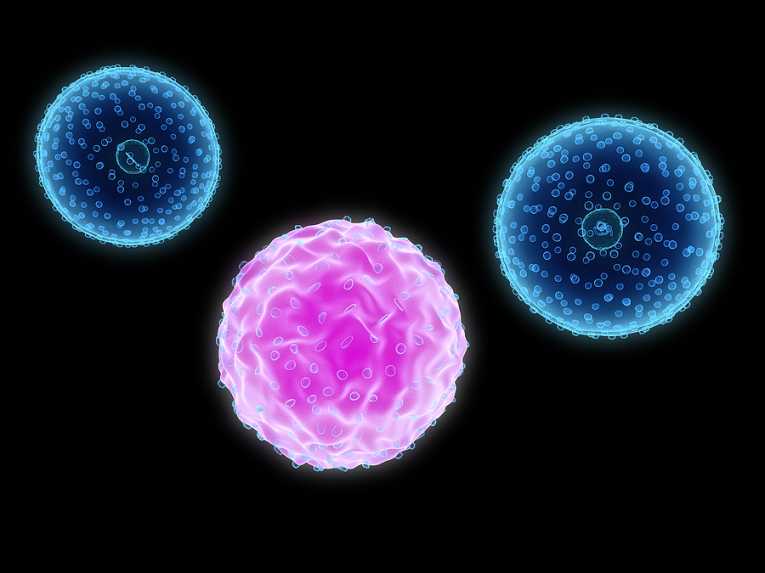
Top Image Credit: 3d render of isolated leukemia cells ©